The characteristics of inflammation
Inflammation is a physiological protective mechanism that our body uses to respond to an external insult and to try to survive it.
Starting from the first description “calor, rubor, tumor, dolor et functio laesa” (heat, redness, swelling, pain, functional alteration) [1], today we know that inflammation is an extremely complex process, as it requires intervention of many cell types that COMMUNICATE AND COORDINATE through the production of signaling molecules, with the aim of eliminating the damaging agent, repairing the damage and returning to the initial state of equilibrium (which is defined as allostatic).
INFLAMMATION IN ITSELF MUST NOT BE CONSIDERED A DISEASE, but a necessary physiological response that helps us to react to an external event, which is a pathogen but also a “stressful” factor allowing our body to adapt to the new reality and regain balance. It is for this reason that we must be sure that the inflammatory process works perfectly.
The cells of the immune system and the stages of inflammation
All the organs of our body host or are located in the immediate vicinity of “sentinel posts” where the cells of the immune system are stationed ready to intervene in case of need. For example, in a previous article we saw how the intestinal epithelium is physically and functionally integrated to an immune barrier structured in various levels of protection (physical, chemical and cellular).
When necessary, intervention on the site of the infection of the cells of the immune system is a rapid and well-marked event in its phases, the beginning and the end. In fact, the response that our organism puts in place in case of need is so powerful and destructive that it must be carefully controlled and limited, both in time and in space, since, otherwise, it can destroy the tissue that it was originally supposed to protect.
The two phases of inflammation, that of ACTIVATION and that of RESOLUTION are closely related to each other by a relationship of dependence: the correct start of the first determines, at the appropriate time, the start of the second and , with it, tissue repair and regeneration.
Both these phases are carried out by the same cell types: neutrophils, macrophages, cells of the extracellular matrix, cells of the vascular endothelium, T lymphocytes, B lymphocytes. Each of these cells has an immunoregulatory role that is not defined a priori, but depends on from the signaling molecules present in the space in which it acts, some with a pro-inflammatory action, others with an anti-inflammatory/resolving action.
A classic example is that of the macrophage, a cell of the immune system responsible for “eating” other cells, it is able to eliminate debris, dead cells and pathogenic cells (proinflammatory macrophage so called “M1”), and then stimulate the formation of new cells and new vascular tissue in the tissue regeneration phase (anti-inflammatory macrophage “M2”)
The failed resolution of the inflammation
As in any biological process, the watchword is balance and control. Since the goal of the acute phase is to eliminate the injuring agent and clean the “battlefield”, once the threat has been eliminated, the intervention of the cells of our immune system must stop. The inability of our body to turn off the inflammatory process is the result of the imbalance between inflammatory activation and resolution and is one of the main causes of the onset of chronic diseases such as rheumatoid arthritis, systemic lupus erythematosus, chronic obstructive pulmonary disease (COPD ) or atherosclerosis.
In addition, in recent decades, it has been observed that certain social, environmental and even behavioral factors are related to the weakening of the inflammation resolution phase, thus leading to an increase in the incidence of pathological states linked to a condition of chronic inflammation. (i.e. prolonged over time) of low grade.
A chronic inflammatory state at a systemic level is therefore configured as a risk factor for cardiovascular and dyslipidemia pathologies and, due to the molecular and cellular mechanisms involved that we know today, an increase or aggravating factor in the immune (and autoimmune), degenerative and metabolic states (picture [2])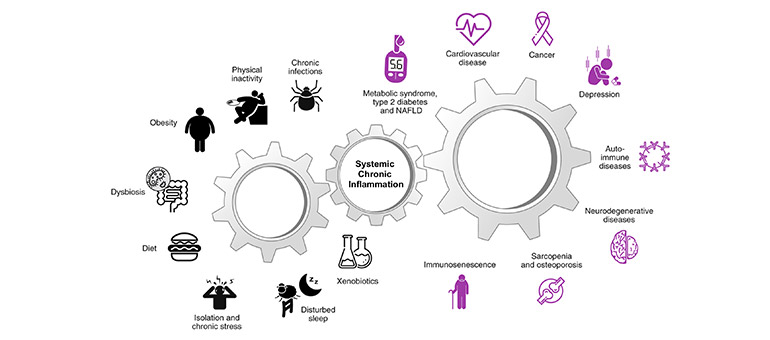
It is (also) a question of fat
With a view to prevention, but also to support treatment in pathological states, we can certainly act on several fronts through appropriate changes to our lifestyle. This is to prevent the systemic chronic inflammation gear from setting in motion.
One of these fronts is represented by food choices, especially in controlling the intake of fats with the diet since they are the precursors of the signaling molecules with which the cells of the immune system communicate in the various inflammatory phases.
– SATURATED FATTY ACIDS: our body can synthesize saturated fatty acids if needed, so in general, there is no need to take them from the diet. Excessive consumption of saturated fats acts directly by promoting inflammation through molecular mechanisms of innate immunity very conserved during evolution.
– OMEGA-6 FATTY ACIDS: they are considered proinflammatory since the proinflammatory molecules of the acute inflammatory phase are synthesized from arachidonic acid.
> Beware of generalizing! Arachidonic acid also generates the STOP inflammation signal (a molecule called Lipoxin A4), so it is extremely crucial that arachidonic acid is present in cell membranes in adequate quantities, neither too much nor too little.
Furthermore, in the omega-6 family there is also dihom-gamma-linolenic acid (DGLA) which has different roles in regulating the balance of pro/anti-inflammatory response as well as in the ability of our immune cells to react in case of need.
– OMEGA-3 FATTY ACIDS (EPA and DHA): these are the precursors of inflammation-resolving molecules with the evocative name of protective and resolving (protectine e resolvine).
> Beware of generalizing! Their central role in resolving inflammation can make us confuse and think that omega-3s are the panacea for any disorder. In fact, the intake of omega-3 without there being a real need creates strong imbalances both in the immune protection system and in the redox balance of the tissues.
Aim for membrane equilibrium
The balance, in terms of quantity and type of fatty acids must be studied in cell membranes since it is from there that cells take DGLA, arachidonic acid, EPA and DHA and transform them into pro-inflammatory signaling molecules or resolution. The balance in the membrane results in an adequate inflammatory response.
[1] Celsus Aulus (Aurelius) Cornelius (30 a.C.-45 d.C) e Claudius Galenus (129 d.C—ca. 200 d.C.)
[2] Figure adapted from Furman D. et al. Nat Med. (2019) 25(12): 1822–1832
To know more:
BOOK: Dalla parte dei grassi. Lipidomica in cucina; perché i grassi non sono tutti uguali e dobbiamo conoscerli “by Dr. Carla Ferreri, Senior Researcher at CNR and Scientific Director of Lipinutragen
Article by the editorial team of Lipinutragen
The information given must in no way replace the direct relationship between health professional and patient.
Photo: 20902133 : @pogonici / 123rf.com