
SEX-BIAS IN AUTOIMMUNITY
Autoimmune diseases include more than 80 chronic diseases that affect almost 5% of the population in Western countries with serious and disabling effects on the quality of life of those affected.
These diseases can affect virtually every organ and tissue, such as the endocrine system, connective tissue, gastrointestinal tract, heart, skin, and kidneys.
The most common autoimmune diseases are systemic lupus erythematosus (SLE), multiple sclerosis (MS), type 1 diabetes, autoimmune thyroid disease, myasthenia gravis, rheumatoid arthritis and inflammatory bowel disease (IBD) such as Crohn’s disease and ulcerative colitis.
The prevalence of autoimmunity in the female gender
The high prevalence in women is a reoccurring and significant aspect: it is estimated that about 80% of affected people belong to the female gender.
From the scientific literature, it is possible to acquire the proportion of incidence by gender:
- the most compelling difference is found in Sjogren’s syndrome (ratio of women: men equal to 16: 1), in SLE (9: 1) and in autoimmune thyroid diseases (Hashimoto 19: 1; Graves 7: 1)
- in rheumatoid arthritis, MS and myasthenia gravis, the ratio of women to men is 2-3: 1
- the difference between the two genders in IBD and type 1 diabetes is negligible
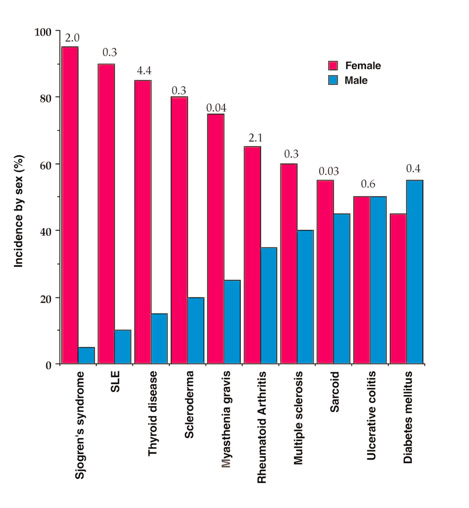
[figure from Whitacre CC. (2001)]
It is interesting to note that the higher incidence among women than men of autoimmune disorders of the connective tissue (such as rheumatoid arthritis, SLE and scleroderma) is observed in the period between late adolescence and 50 years, with a relevant peak in the decade 41-50, coinciding with major changes in hormone levels in women.
With the arrival of menopause, the gender difference fades and, in the case of rheumatoid arthritis, after the age of 75 the incidence is higher in men.
This epidemiological evidence has for many years directed studies on the influence of hormones in determining the risk of disease, due to the hormonal fluctuations to which women are exposed throughout their life.
Likely, gender hormones such as estrogen, androgen, progesterone, and prolactin, can mediate most of the differences in sex-related immune responses. However, the picture is probably more complex and must be sought in the interactions between genetic, hormonal and environmental factors.
Hormonal risk factors
Females have greater immuno-reactivity than males, with higher immunoglobulin levels and higher antibody production upon stimulation by antigens.
Overall, therefore, women activate more powerful and effective immune responses, but, for the same reason, they have a greater susceptibility to autoimmunity.
Estrogens and androgens directly influence the development of a Th1 or Th2 type immune response by interacting with hormone receptors present in immune cells.
At the same time, the cells of the immune system, through the production of cytokines, can regulate the production of sex hormones, suggesting a bidirectional regulation of the immune response.
In general:
- estrogens, in particular 17-β estradiol, act as dose-dependent immunomodulators. At high doses, such as during pregnancy, estrogens have an anti-inflammatory effect (to ensure mother-fetus immune tolerance), while at low doses they have a pro-inflammatory effect;
- androgens act as natural immunosuppressants;
- progesterone has an anti-inflammatory effect.
In women, estrogen and progesterone levels decrease as menopause approaches.
This could, at least in part, explain the high ratio of women: men in the onset of some autoimmune diseases in the period of perimenopause (conventionally between 40 and 50 years).
The protective action of androgens has been demonstrated in studies showing that men with rheumatoid arthritis have significantly lower testosterone levels. Similarly, men with low serum cortisol and low testosterone levels are at an increased risk of developing rheumatoid arthritis.
The role of sex hormones, however, is not simple and undemanding. Susceptibility to autoimmune diseases can be the result of a complex interaction and balance between all hormones which, on the other hand, have the same precursor: cholesterol.
Gene-environment interaction: the integrity of barriers
Genetics play a key role in predisposition to autoimmune diseases.
In a genetically susceptible individual, exposure to environmental factors (such as sunlight, diet, allergens, infectious agents, or environmental toxins) can act to initiate an autoimmune process.
The combined effects of genes and the environment occur at the level of the body’s mucous membranes. Skin, eyes, nasal / oral mucosa, lungs, urogenital and gastrointestinal tracts act as protective barriers against the physical, chemical and microbial agents.
For this reason, most of the body’s immune cells are associated with mucous membranes.
The cells of these “barrier” tissues must maintain the integrity of their cell membrane, there must be no deficiencies in essential elements, such as polyunsaturated fats, to maintain the organization of the membrane and regulate inflammatory and immune responses.
The alteration of the integrity of the barrier systems, affecting their structure (with increased permeability) or functions (for example, in the intestine, inducing the alteration of the commensal microbial population), can in fact lead to an “exaggerated” inflammatory response in acquaintance with any type of agent, and this can trigger or perpetuate the autoimmune process in those particularly sensitive or predisposed subjects.

Nutrition provides for the supply of essential elements, the ones that are, not prepared by the human body but essential for the formation of its cells.
But if the diet is not balanced, for example it does not provide essential fats, it can lead to a precarious condition at the epithelial cellular level and in the regulation of inflammatory processes.
In fragile subjects these deficiencies must be carefully avoided, and a check-up with membrane lipidomic analysis becomes a necessary control tool.
Learn more on Lipimagazine:
To deepen on the scientific literature:
Whitacre CC. Sex differences in autoimmune disease. Nat Immunol. 2001 Sep;2(9):777-80. https://doi.org/10.1038/ni0901-777
Rainer H. Straub ” The Complex Role of Estrogens in Inflammation” Endocrine Reviews, Volume 28, Issue 5, 1 August 2007, Pages 521–574, https://doi.org/10.1210/er.2007-0001
Oliver, J.E., Silman, A.J. Why are women predisposed to autoimmune rheumatic diseases?. Arthritis Res Ther 11, 252 (2009). https://doi.org/10.1186/ar2825
Article by the editorial team of Lipinutragen
The information provided must in no way replace the direct relationship between health professional and patient.
The food recommendations in the article are not intended as a substitute for a personalized meal plan and are to be adapted to specific cases
Photo: 123RF Archivio Fotografico: 69266179 : ©mandameeca | 65512027 : ©kerdkanno
- On 18 May 2022



